
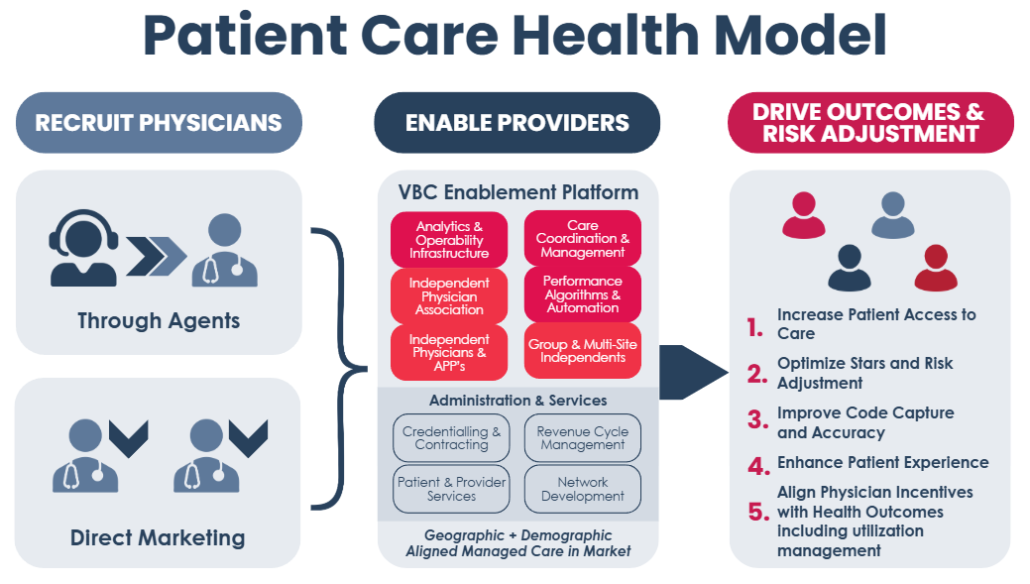
Enabling Patient-Centered Value-Based Managed Care in Optimized Provider Networks.
PCH offers Medicare and ACA carriers a unique experience for their members’ access – providers optimized to execute value-based, patient-centered managed care.
Our extensive experience delivering value-based consultations to independent healthcare providers provides these opportunities to access:
- A broad network of experienced, well-trained insurance agents to convert Medicare and ACA panels at providers to your plans as needed.
- Using call centers on patient outreach to provide reminders for upcoming care visits, notice that a preventive test or exam is due and to help schedule visits.
- Enable Value Based Care in ACA and Medicare by aligning services and partnerships that deliver performance to health plan objectives including:
- Risk Adjustment
- Utilization Management
- Coding training and expertise to national and carrier standards pinpointing issues needing correction and opportunities for member engagement and experience optimization
- Quality & Outcomes Improvements
- Value-based arrangements including P4P, Episodic, Shared Savings (Gainshare) and for care coordination.
- Focus on the Plan Liability Risk Score (PLRS) through Dx, Rx, HCC Coding
and Severity Factor Reporting.
- Compliance expertise in the ACA and Medicare worlds assisting healthcare providers be compliant with CMS, ACA, Medicare and carrier regulations on all needed aspects of business.
- Coordinating appropriate utilization of care from enrollment through screens to health condition capture and ongoing care management.

Join Our Network!
PCH offers tools and technology for carriers’ independent healthcare practitioners to access new high-value patient acquisitions with innovative retention strategies.

